Perimenopause Care
at Bridged Connections Psychiatry
Perimenopause is more than hot flashes — we’re here to support the whole you.
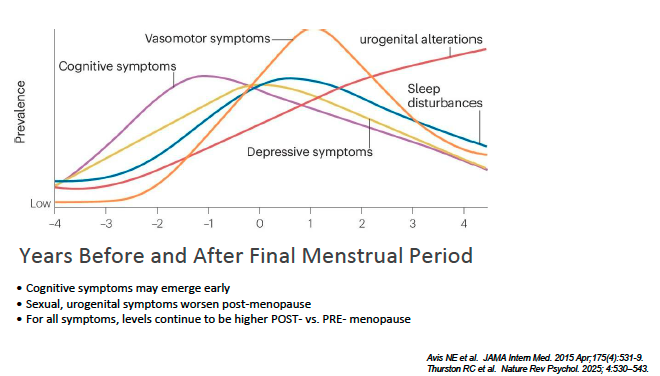
From brain fog and mood swings to sleep struggles and body changes, perimenopause can feel overwhelming.
At Bridged Connections, we help you navigate this transition with compassion, expertise, and personalized care.

Perimenopause 101
Perimenopause is the transition leading up to menopause, often starting in your 40s (sometimes earlier).
Estrogen and progesterone levels fluctuate, creating a rollercoaster of symptoms.
-
The uterine lining is shed — this is your period. Estrogen and progesterone are at their lowest, which can bring cramping, fatigue, and mood changes.
-
FSH (Follicle-stimulating hormone) rises and stimulates ovarian follicles. Estrogen increases, thickening the uterine lining. Energy, mood, and focus usually improve during this phase.
-
An LH (lutieinizing hormone) surge triggers the release of an egg. Estrogen peaks and progesterone begins to rise. Many notice an increase in libido and fertile cervical mucus.
-
After ovulation, the follicle that released the egg turns into a little gland called the corpus luteum. Its job is to make progesterone, the hormone that prepares the body for a possible pregnancy—and in sensitive brains, those hormone changes can trigger PMS or PMDD symptoms.
If pregnancy doesn’t occur, hormones drop, and bleeding begins again.
-
PMDD (Premenstrual Dysphoric Disorder) symptoms occur only in the luteal phase and clear once bleeding starts. This cyclical pattern is what makes PMDD different from conditions like bipolar disorder, which is not cycle-dependent.
The Four Phases of the Menstrual Cycle
-
What it can feel like: Word-finding slips, losing your train of thought, slower recall, mental “static.”
How it impacts daily life: Missed details at work, re-reading emails, longer time to complete tasks, second-guessing decisions.
Self-care / when to call: Prioritize sleep, reduce multitasking, use lists; if memory loss is sudden/worsening or affects safety, seek medical care.
-
What it can feel like: Restlessness, feeling “on edge,” short fuse, physical tension.
How it impacts daily life: Conflict at home/work, avoidance of tasks, decision paralysis, poor sleep.
Self-care / when to call: Mindfulness, weekly massages, structured routine, exercise; reach out if anxiety interferes with work/relationships or includes panic.
-
What it can feel like: Persistent sadness, loss of interest, guilt, low energy, tearfulness.
How it impacts daily life: Social withdrawal, decreased productivity, skipped self-care, appetite/sleep changes.
Self-care / when to call: Social support, sunlight/activity; seek care if symptoms last >2 weeks, include hopelessness, or any thoughts of self-harm (urgent help immediately).
-
What it can feel like: Trouble falling or staying asleep, 3–4 a.m. wakeups, unrefreshing sleep.
How it impacts daily life: Daytime fatigue, fog, mood swings, reduced pain tolerance.
Self-care / when to call: Consistent wake time, cool room, limit evening alcohol; ask about CBT-I and treatments for hot flashes.
-
What it can feel like: Sudden heat, flushing, pounding heart, then chills; bed-soaking sweats.
How it impacts daily life: Sleep loss, wardrobe changes, embarrassment in meetings, avoidance of social events.
Self-care / when to call: Layering, fans, cooling pillow; discuss hormone and non-hormone options if frequent or sleep-breaking.
-
What it can feel like: Cycle length swings, surprise bleeding, very heavy days, clots.
How it impacts daily life: Anxiety about leaks, missed work, iron deficiency fatigue.
Self-care / when to call: Track cycles; seek care for flooding, clots > quarter-size, bleeding >7 days, or bleeding after 12 months without periods.
-
What it can feel like: Intensified premenstrual mood swings, rage, hopelessness, severe irritability.
How it impacts daily life: Conflict, missed responsibilities, distress during luteal phase.
Self-care / when to call: Luteal-phase tracking, nutrition, sleep; ask about targeted treatments (including SSRIs, CBT, or hormone approaches).
-
What it can feel like: New or worse cyclical headaches; light/sound sensitivity, nausea.
How it impacts daily life: Time off work, screen intolerance, reduced exercise.
Self-care / when to call: Hydration, regular meals, sleep; seek care for “worst headache,” new neuro symptoms, or change in pattern/frequency.
-
What it can feel like: Morning stiffness, achy hands/knees/hips, “creaky” feeling.
How it impacts daily life: Slower mornings, exercise avoidance, reduced grip strength.
Self-care / when to call: Gentle strength training, stretching, anti-inflammatory nutrition; evaluate if swelling, redness, or functional loss.
-
What it can feel like: Skipped/strong beats, lightheadedness, brief spins (often with hot flashes).
How it impacts daily life: Anxiety, activity avoidance, fear of exercise.
Self-care / when to call: Hydration, limit caffeine/alcohol; urgent care for chest pain, fainting, shortness of breath, or persistent palpitations.
-
What it can feel like: Vaginal dryness/itching, burning, tearing, pain with penetration; urinary urgency or recurrent UTIs.
How it impacts daily life: Avoidance of intimacy, pelvic discomfort, sleep interruption from urinary symptoms.
Self-care / when to call: Regular moisturizers/lubricants; ask about vaginal estrogen or DHEA for long-term relief (safe and low-dose local).
-
What it can feel like: Lower desire, delayed arousal, less pleasure; sometimes increased irritability around intimacy.
How it impacts daily life: Relationship strain, avoidance, reduced closeness.
Self-care / when to call: Pain-free sex (treat GSM), schedule intimacy, communicate needs; discuss medical/psych options if distressing.
-
What it can feel like: Dry/itchy skin, scalp changes, shedding hair; ear itching, burning mouth, altered taste; dry eyes.
How it impacts daily life: Discomfort, distraction, self-consciousness, dental sensitivity.
Self-care / when to call: Gentle skincare, humidifier, hydration; dental/ENT eval if persistent or painful; treat dryness (e.g., vaginal/ocular as needed).
-
What it can feel like: Easier fat gain (especially abdominal), harder to build muscle, energy dips after meals.
How it impacts daily life: Frustration, body-image concerns, decreased stamina.
Self-care / when to call: Protein with each meal, fiber, resistance training, daily movement; discuss thyroid, iron, glucose/lipids if concerned.
-
What it can feel like: Fatigue, hair changes, temperature sensitivity—can overlap with perimenopause.
How it impacts daily life: Confusion about what’s causing what, delayed care.
Self-care / when to call: Get a medical review—sometimes checking TSH and iron/B-12 clarifies the picture.
-
Call 911/urgent care for: Chest pain, trouble breathing, one-sided weakness/numbness, severe new headache, fainting, heavy uncontrolled bleeding, or thoughts of self-harm.
Perimenopause Symptoms
Our Approach to Symptom relief
Family-Centered, Whole-Person Care
Personalized Psychiatry:
Evidence-based prescribing, including safe hormone therapy integration when appropriate
Integrative Wellness:
Nutrition, supplements (like Omega-3s, vitamin D, DHEA), and lifestyle strategies
Collaborative Care:
We partner with OB-GYNs, primary care, and therapists for holistic support
Safe Space:
We honor your lived experience — no symptom is “too small” or “too strange.”
-
Portable neck fans or small handheld fans can help manage hot flashes and night sweats. Keep one in your bag or bedside table for quick relief.
-
-
-
Deep breathing, meditation apps, or even short stretches can lower stress hormones and reduce the intensity of symptoms.
-
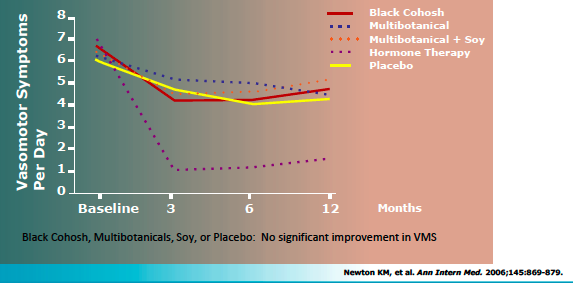
Plant estrogens found in soy or red clover. May modestly reduce hot flashes for some, especially in early menopause. Results vary, and benefits are usually mild.
-
An herbal supplement sometimes used for hot flashes. Research is mixed. Long-term safety is uncertain, so use with caution and under guidance.
-
Important for bone health after menopause. Doesn’t treat hot flashes directly, but many women are low in vitamin D. Good baseline support.
Tip: Aim for food sources first (dairy, fortified plant milks, leafy greens, fish), and supplement only the gap.
-
Role: Vitamin K2 (menaquinone) helps with bone metabolism (guides calcium into bone rather than soft tissue).
Evidence: Some small studies suggest added benefit for bone density, but NAMS does not formally recommend routine Vitamin K supplementation for all menopausal women.
When to consider: If patient is already low in K (rare in a balanced diet) or under endocrinology guidance.
Caution: Avoid supplementing Vitamin K without oversight in patients on anticoagulants (e.g., warfarin).
-
B6, B12, folate, and riboflavin may help with energy and mood in general, though research specific to menopause symptoms is limited.
-
Can support mild mood symptoms. May interact with many medications (antidepressants, anticoagulants, etc.), so check with a provider before use.
-
Lavender oil capsules (like the standardized product Silexan) have shown benefit in clinical studies for mild to moderate anxiety.
May support stress, mild anxiety, and sleep.
Evidence is stronger in general anxiety, not specifically perimenopause.
Safety: usually well tolerated, but can interact with sedatives, SSRIs, or anticoagulants.
Tip: If you try it, use a standardized capsule, track symptoms for 6–8 weeks, and check with your provider first.
🌡️ Symptom Hacks & Relief Tools
What the research tells us about supplements. The results are close to placebo. Some may benefit, but for the vast majority will not.

Tips, Tricks, and Partner Resources
-
Hormone shifts can affect mood, sleep, and energy. These changes are real and can feel unpredictable. Some days are fine; others feel overwhelming.
-
• Irritability or “short fuse”
• Sadness or tearfulness
• Anxiety or restlessness
• Sleep problems (which amplify symptoms)
• Feeling overwhelmed or less patient -
• Listen without trying to fix
• Validate (“I can see this is really hard”)
• Share the load (meals, chores, kids)
• Protect rest/sleep time
• Remember: it’s not personal—it’s hormones
• Join healthy habits (walks, stretching, mindfulness) -
• Severe/frequent mood swings or major conflict
• Hopelessness, panic attacks, losing interest in life
• Your partner wants support (therapy, lifestyle tools, or medical options) -
Perimenopause is a shared journey. Patience and compassion can lower stress and strengthen your connection.